Kinesiology: On the frontline of the battle against cardiovascular disease.
Illustration by Alex Nabaum
Cardiovascular disease is the leading cause of death worldwide, and the risk is higher for certain populations. For example, heart disease is the number one killer of women, and hypertension-related ailments account for 20 percent of all deaths among African-Americans. Over one-third of adult Americans are obese and face increased risk of cardiovascular disease.
Whether it’s hypertension, heart attack, or stroke, the College’s Department of Kinesiology has built a team of researchers who are working to better understand the mechanisms underlying these cardiovascular diseases. The team’s ultimate goal is to discover novel therapeutic strategies that combat these life-threatening conditions.
“We’ve got the cardiovascular system covered,” says Michael Nelson, assistant professor of kinesiology.
Dr. Nelson joined the department last year and is studying root causes of heart disease in women. The new and growing team also includes Associate Professor Matthew Brothers, who joined the college last year from UT Austin. His work focuses on mechanisms of impaired vascular function known to be present in populations with cardiovascular disease. And in 2015, the department hired Paul Fadel, a prominent integrative physiology researcher and expert in neural cardiovascular control. Dr. Fadel also serves as the College’s associate dean for research and director of clinical translational science. In 2016, he was awarded a $1.7 million grant by the National Institutes of Health to study the role of the autonomic nervous system in cardiovascular disease and high blood pressure in patients with chronic kidney disease. Fadel is also working with David Keller, associate dean and chair of the Department of Kinesiology, on a study that investigates differences in vascular responses in blacks and whites in blood pressure regulation. The Kinesiology Department’s recent recruit, Rhonda Prisby, studies the interaction between blood vessels and bone. Recently she received an American Heart Association grant to investigate how inflammation in the bone marrow contributes to blood vessel dysfunction, loss of patency, and arterial emboli.
These experts work individually and collaboratively, making a team that together has been awarded millions of dollars in grants from sources such as the National Institutes of Health and the American Heart Association. It’s the kind of innovative research that contributes to one of the pillars of UTA’s Strategic Plan 2020: Bold Solutions | Global Impact: improving health and the human condition.
The Vascular Expert
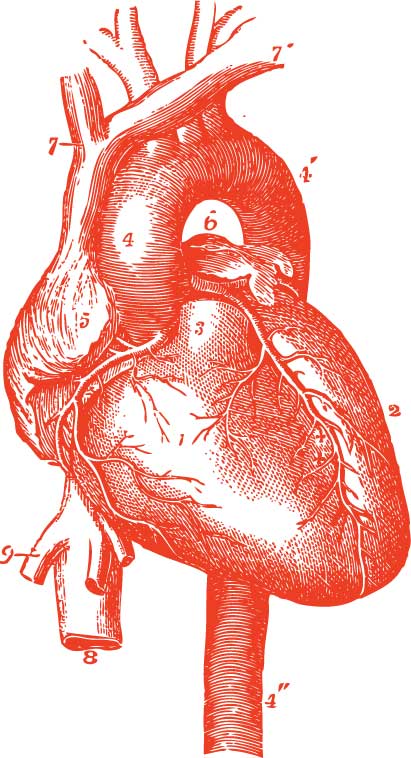
The cardiovascular system has thousands of miles of arteries and veins that deliver oxygen and nutrients to every cell, carting away carbon dioxide and waste along the way. It functions because the heart and peripheral blood vessels are working together.
Dr. Brothers is pursuing several studies on blood vessel function and implications in a variety of conditions, such as strokes, hypertension and Type-2 Diabetes.
“This work may shift the paradigm of our approach in treating such diseases.”

Dr. Matthew Brothers
“There are many reasons for heightened risk,” says Brothers. “We’re trying to identify the potential reason why blood vessels aren’t functioning properly. The next step is to identify some life style interventions to delay the progression and hopefully reverse this dysfunction.”
African-Americans and obese individuals experience higher rates of heart disease. A primary problem for these populations is dysfunction of blood vessels in the brain and other vascular beds. Brothers’ research focuses on how blood vessels function and what makes vessels dilate or not. Impaired dilation of vessels can lead to hypertension, stroke, atherosclerosis, and heart attacks.
An ongoing area of investigation in Brothers’ lab is the role of oxidative stress in impaired brain and peripheral blood vessel function. Work recently published by his group shows the therapeutic potential of antioxidant therapy in at-risk individuals.
This work has led to several collaborations between Brothers and Nelson. One such collaboration focuses on the effect of a high fat meal on vascular function. Another study, funded by the Center for Translational Medicine at University of Texas Southwestern Medical Center, is investigating the effect of obesity and subsequent bariatric surgery on brain vascular health and cognitive function.
The Heart Expert
Dr. Michael Nelson is particularly interested in the heart. Nelson—who is also an adjunct professor of bioengineering and a visiting faculty scientist at Cedars-Sinai Medical Center in Los Angeles—is conducting research that could help women with a rare form of heart disease and people whose heart conditions leave them unable to manage simple tasks.
In 2016, he received a four-year, $308,000 grant from the American Heart Association to study the root causes of a condition that damages blood vessels in the women’s heart. Symptoms of this coronary microvascular dysfunction often include chest pain, shortness of breath and fatigue. Diagnoses frequently elude cardiologists, who have traditionally relied on major blockages of blood vessels to dictate clinical courses of action.
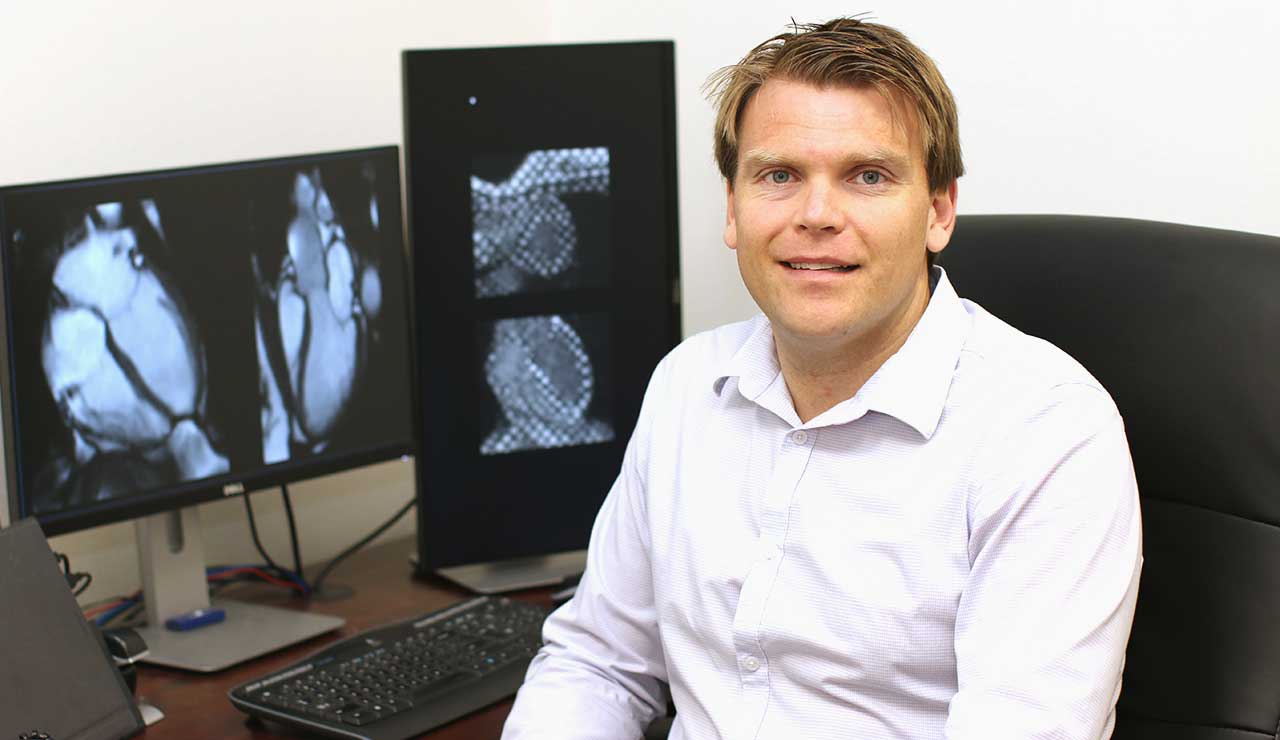
Dr. Michael Nelson
Most women afflicted with the coronary artery condition have several things in common, including risk factors such as diabetes, hypertension, and obesity. Nelson’s previous research has demonstrated that the heart does not relax well in this group.
“Our hypothesis is that the impaired relaxation of the heart is directly related to coronary microvascular dysfunction and contributes to the progression of heart failure,” Nelson says.
He and his team will use MRI techniques to test the hypothesis. This technique allows for optimal assessment of both heart and blood vessel function.
In addition, Nelson is working with several other researchers—Mark Haykowsky, Paul Fadel, and Paul Bhella from the College of Nursing and Health Innovation; Hanli Liu and Fengha Tian from the College of Engineering; and Robert Gatchel from the College of Science—to develop other novel imaging techniques to study blood flow regulation in patients with heart failure. The team received one of four seed grants UTA awarded last August to interdisciplinary research projects.
“This is an incredible cross-discipline collaboration,” Nelson says. “It simply could not be done anywhere else in the world but here at UTA.”
The Bone Expert
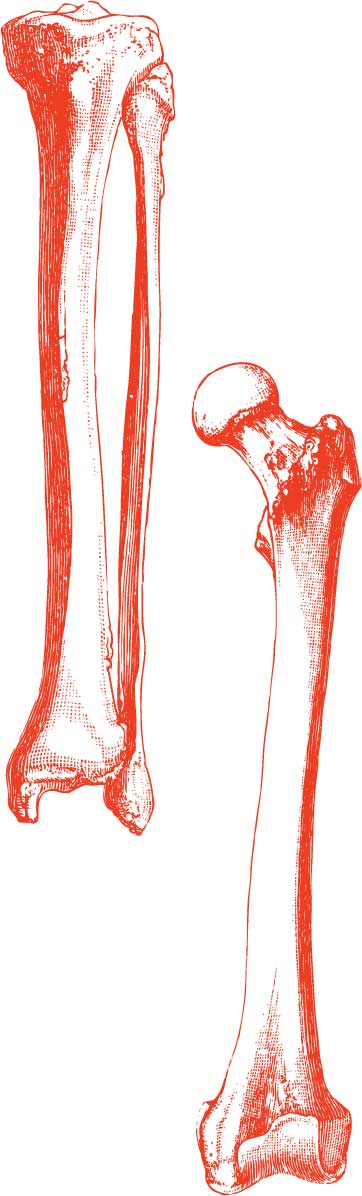
Skeletal tissue is highly vascularized and Dr. Rhonda Prisby is deciphering the interaction between blood vessels and bone in health and disease. Prisby, also an adjunct professor of bioengineering, is conducting research that could aid in the treatment of diseases with low bone mass and impaired fracture healing by examining how blood vessels contribute to bone health or bone decline.
In 2016, she received a two-year, $150,000 Innovative Research grant from the American Heart Association to study the role of inflammation on vascular dysfunction in bone and the generation of bone-like blood particles. Her two recent discoveries—the conversion of blood vessel into bone and bone-like particles in the peripheral circulation of rodents and humans—serve as the basis for this award. The loss of vascular function in bone may lead to impaired delivery of oxygen and nutrients to the skeleton. Circulating bone-like blood particles may contribute to diseases such as heart attack and stroke.
Dr. Rhonda Prisby
“We are looking at whether inflammation in bone marrow contributes to blood vessel dysfunction, the conversion of blood vessels into bone, and the generation of bone-like blood particles,” she says.
Since the diagnosis of vascular pathology within the skeleton is difficult in the clinical setting, Prisby’s research may lead to diagnostic techniques capable of assessing risk of emboli, particularly in those of advanced age.
Prisby will work with several clinical researchers in the Department of Kinesiology, such as Fadel, and the College of Nursing and Health Innovation to further characterize the presence of bone-like blood particles in patients with cardiovascular disease.
“This research is extremely exciting and may alter our understanding of the development of heart and strokes,” Prisby says. “Additionally, this work may shift the paradigm of our approach in treating such diseases.”
The Nerve Experts
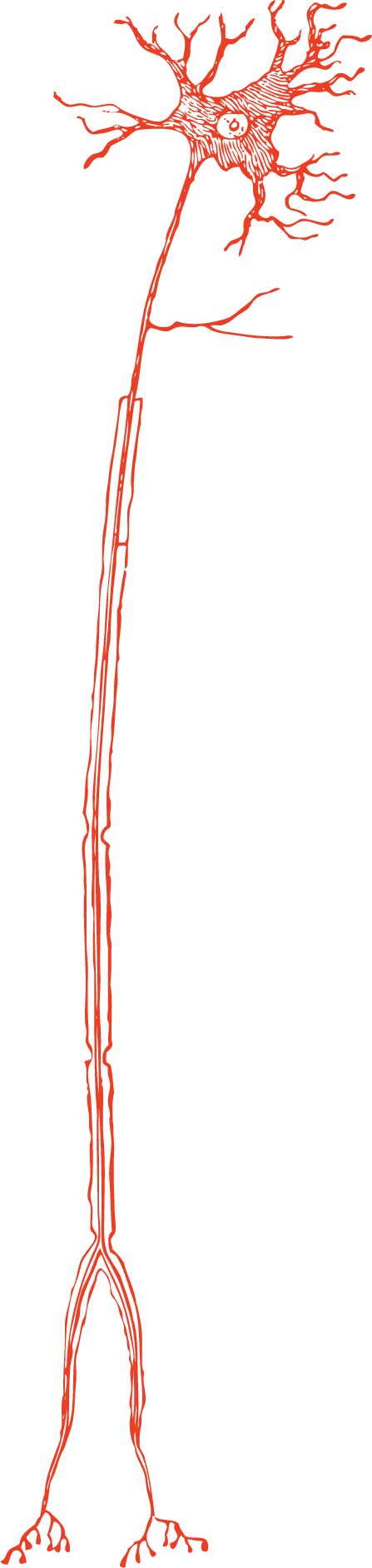
The sympathetic branch of the autonomic nervous system plays a crucial role in controlling the peripheral vasculature. Importantly, impairments in this system contribute to hypertension.
Nearly half of African-American adults are at risk of developing hypertension, a rate significantly higher than that of any other group in the United States.
Keller and Fadel, both experts in neural control of the circulation, are working to address this important issue. Last year, they were awarded a $376,000 National Institutes of Health grant, with which they will investigate differences in vascular responses in blacks and whites in blood pressure regulation both at rest and during exercise. Keller and Fadel say insights gained through their studies will help to better understand the underlying causes contributing to the greater occurrence of hypertension in African-Americans. This work will hopefully contribute to reducing the prevalence of hypertension in this group.

Dr. David Keller and Dr. Paul Fadel
An important aim of this study is to examine the role of family history of high blood pressure. Keller says a thorough understanding of biological mechanisms associated with hypertension in African-Americans could have significant ramifications for all racial and ethnic groups.
The addition of these integrative physiologists in the Department of Kinesiology puts UTA on the cutting edge of basic and applied cardiovascular research in health and disease.
“When you look at what type of work is being funded, there’s much more attention and allocation of resource to teams of investigators working together to solve common problems,” says Keller. “Through our alignment with the University’s strategic themes, our researchers are extremely well-situated for continued success and contribution to the understanding of health and disease across the lifespan.”