Photograph by Adam Voorhes
While studying influenza in 1928, a British scientist noticed that mold had developed on a petri dish in which staphylococci was growing. That scientist was Alexander Fleming, and he had just discovered penicillin, the world’s first antibiotic. One of the greatest advances in medicine, these so-called wonder drugs would save millions of lives over the next century and radically improve the way we treat bacterial infections.
Yet today, an antibiotics crisis looms. A growing number of people are dying from infections and strains of pneumonia, tuberculosis, and other diseases that have become impervious to antibiotics, due partially to the drugs’ overuse. Without action, many modern medicines soon could be rendered completely ineffective.
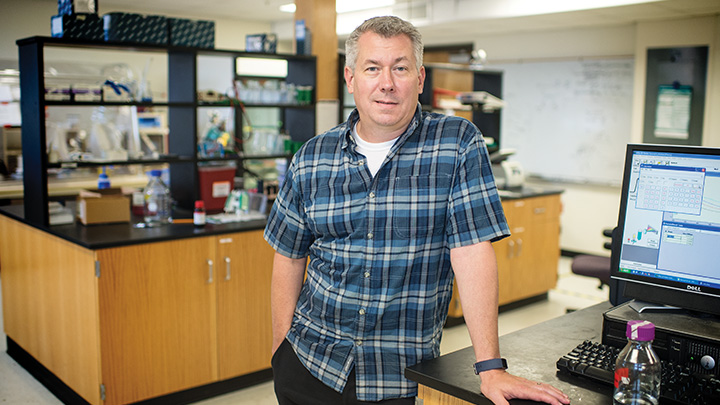
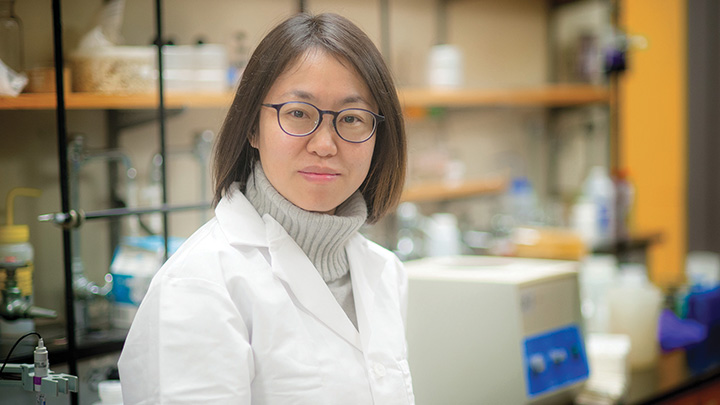
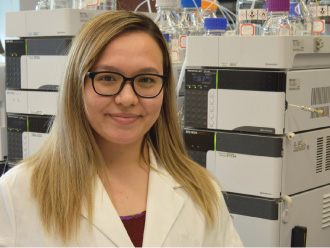
Scientists at The University of Texas at Arlington are addressing the escalating public health issue. Researchers from a variety of fields are harnessing the body’s natural defenses to fight bacteria, studying enzymes to facilitate the development of new drugs, and seeking new and improved ways to treat infections in hospitals and military facilities.
Their research, which has drawn millions of dollars in grants, is urgent. The Centers for Disease Control and Prevention (CDC) warns that antibiotic resistance is one of the most pressing challenges of our time—each year in the United States at least 2 million people fall ill from antibiotic-resistant infections, and some 23,000 people die from them. Further, such infections are associated with close to $20 billion in direct medical costs annually, according to the Alliance for the Prudent Use of Antibiotics.
The crisis extends far beyond the United States. In India, for example, more than 58,000 babies died in one year as a result of infections with resistant bacteria, typically passed on from their mothers.
At UTA, bacteria research got a recent boost with the 2018 opening of the Science & Engineering Innovation & Research building. The $125 million, state-of-the-art facility is helping to push the University forward as a leading health science research and teaching institution. Employing the modern concept of research lab neighborhoods, the facility drives collaboration and creativity across a multitude of disciplines, including science, engineering, nursing, kinesiology, and public health.
“Our research programs on antibiotic resistance are evidence of UTA’s growing expertise in the health science field, as well as the University’s commitment to lead on a national scope,” College of Science Dean Morteza Khaledi says. “Research being done in laboratories here could lead to life-saving breakthroughs that benefit all of us.”